Young Adult Health Solutions: Key Prevention Strategies
Part 3 of a 3-Part Series
Introduction
In Parts 1 and 2 of this series, we established that young adult mortality in the United States is rising and that drug overdose, suicide, and unintentional injury are the primary drivers (Centers for Disease Control and Prevention [CDC], 2023; Hedegaard et al., 2021; National Institute of Mental Health [NIMH], 2023). The most critical question now becomes:
What can be done to reverse these trends?
1. Strengthening Behavioral Health Access
Behavioral health must become a foundational component of primary care, not a secondary referral (Substance Abuse and Mental Health Services Administration [SAMHSA], 2022). Evidence-based strategies include:
- Expanded tele-behavioral health services
- Integrated primary and behavioral health teams
- Crisis intervention alternatives to emergency departments
- Workforce investment in counselors, social workers, and addiction specialists
These strategies reduce emergency utilization while improving long-term treatment engagement (SAMHSA, 2022).
2. Modernizing Substance-Use Prevention and Treatment
Overdose deaths are preventable through proven interventions, including:
- Widespread naloxone distribution
- Medication-assisted treatment (MAT)
- Long-term recovery housing
- Removal of stigma-based access barriers (CDC, 2023)
Treating substance use disorder as a chronic medical condition rather than a moral failing is essential for sustainability (CDC, 2023; Hedegaard et al., 2021).

Figure 5. Preventable vs. Non-Preventable Young Adult Deaths (Modeled Estimate)
Source: CDC cause-of-death patterns & SAMHSA prevention benchmarks
3. Injury and Violence Prevention Initiatives
Healthcare systems can reduce injury-related deaths through community-level prevention programs, including:
- Impaired- and distracted-driving prevention campaigns
- Firearm safety counseling
- Workplace injury prevention education
- Youth violence prevention partnerships (CDC, 2023)
These interventions directly reduce trauma-system burden and prevent years of potential life lost (Rockett et al., 2018).
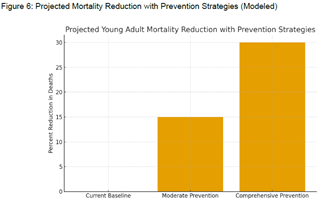
Figure 6. Projected Young Adult Mortality Reduction with Prevention Strategies (Modeled Projection)
Source: Population health intervention benchmarks
4. Addressing Social Determinants of Health
Long-term mortality reduction is impossible without addressing non-medical drivers of health, including:
- Housing stability
- Food access
- Education attainment
- Employment opportunity
- Transportation access (World Health Organization [WHO], 2022; National Academies of Sciences, Engineering, and Medicine, 2019)
Healthcare organizations increasingly play a direct role in screening for and addressing these risk factors.
5. Data-Driven Population Health Strategy
Sustainable prevention requires:
- Real-time mortality and injury surveillance
- Community-level analytics
- Employer and payer engagement
- Cross-sector collaboration between healthcare, education, justice, and social services (SAMHSA, 2022; CDC, 2023)
Conclusion
Rising mortality among young adults represents one of the most urgent public health failures of our time—yet it is also one of the most preventable (CDC, 2023; WHO, 2022).
Healthcare leaders, consultants, and policymakers now face a defining question: Will systems continue reacting to crisis—or move decisively toward prevention, equity, and long-term sustainability?
The path forward is clear. The responsibility is collective. And the opportunity to save lives is immediate.
End of 3-Part Series
References
Centers for Disease Control and Prevention. (2023). Overdose prevention and deaths and mortality.
Hedegaard, H., Miniño, A. M., & Warner, M. (2021). Drug overdose deaths in the United States, 1999–2020. National Center for Health Statistics Data Brief No. 428.
National Institute of Mental Health. (2023). Suicide statistics.
Rockett, I. R. H., Smith, G. S., Caine, E. D., Kapusta, N. D., Hanzlick, R. L., Larkin, G. L., … Miller, T. R. (2018). Causes of death among young adults in the United States. American Journal of Preventive Medicine, 54(1), 1–11.
Substance Abuse and Mental Health Services Administration. (2022). Key substance use and mental health indicators in the United States.
World Health Organization. (2022). Social determinants of health.
National Academies of Sciences, Engineering, and Medicine. (2019). Integrating social care into the delivery of health care: Moving upstream to improve the nation’s health. National Academies Press.
